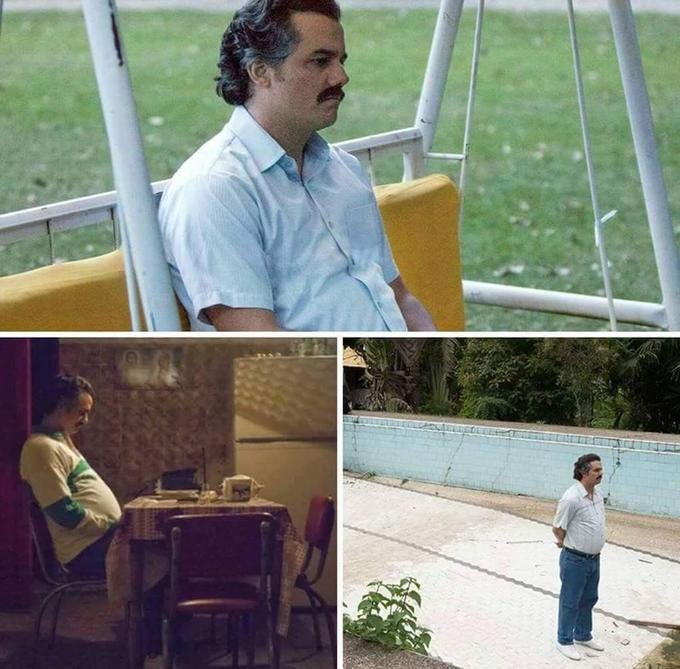
I recently had a chance to chat with Vijay Pande, Justin Larkin, and Sonal Chokshi at Andreessen Horowitz about digital therapeutics. They were looking for experts but all of them were busy, so they found a person that makes healthcare memes instead. The podcast comes out just as Akili, a video game to treat ADHD, had been approved by the FDA. Here’s the link to the podcast if you’re interested. Since there’s no commute to work, you can listen in your house like:
I wanted to go over and elaborate some of the major points that came up during the podcast.
What is a digital therapeutic?
I think it’s illegal to talk about digital therapeutics without debating what the definition of it actually is. There’s a million pieces written by much smarter people than myself about what constitutes a digital therapeutic, so go read those.
What’s generally agreed upon is that it’s some sort of software that is clinically-validated through a trial/study, and targets a specific endpoint (e.g. blood sugar level, Attention Performance Index to measure ADHD, etc.). HOW that happens is generally up for debate. The general debate is which of these buckets is a digital therapeutic:
Bucket 1: The software alone creates a therapeutic effect. Akili, which was a recently approved by the FDA as a video game to treat ADHD, has a measurable clinical effect on attention span with the software alone. There are lots of companies that combine virtual reality with software to do things like address pain management, depression, etc.

Bucket 2: The software gets a patient to do a certain behavior that results in a clinical outcome. Proteus, which was a smart pill combined with a drug to increase compliance, would fall into this bucket. Also in this bucket would be companies target musculoskeletal issues by issuing series of exercises and measuring a patients mobility/pain at the end of a defined time period.
Bucket 3: Software AND services (coaches, doctors, peers, etc.) enable a change in patient behavior within a specific time period to change some measurable biomarker. Virtual diabetes prevention programs over the course a few months to manage blood sugar levels and drop weight would be an example.
In general, I think we’ve spent a cumulative $3.6T in man hours debating this as an industry. But it’s important because the term “therapeutic” actually has importance when it comes to the amount of evidence you need to back it up, who gives it to patients, and how you charge for it.
In the podcast we debate what should count, but right now I’m in the camp that only bucket 1 actually counts as a “therapeutic”. The other ones are definitely valuable, but to call them therapeutics by themselves is probably a stretch.

Bucket 2 companies that combine software with an actual drug are complements that should be packaged with the drug to drive better outcomes, I wouldn’t call them therapeutics by themselves.
Bucket 2 companies that automate content + nudges to get patients to do things are patient engagement platforms IMO.
Bucket 3 companies are just a different form of telemedicine.
But I think the reason we keep trying to create these buckets and specific definitions is because we haven’t figured out how to actually think about how digital therapeutics should be priced and distributed.
Digital Therapeutics and Pricing
This conversation highlights a parallel issue happening in healthcare: how do we move to a system that prices for how good the drug is as opposed to the number of units that drug sells? Aka. moving to outcomes-based pricing for drugs.
I think digital therapeutics are just another proof point that we need to move past our current volume-based “number of units sold” pricing model and into an outcomes-based “did it actually work?” one.
The concept of pricing tied to volume has become outdated now that we have extremely expensive one-shot cures like Zolgensma and digital therapeutics which have near 0 marginal cost to giving one more “dose”. Plus with more real-world data we can better track outcomes and understand (imperfectly) how to attribute those outcomes to interventions/new therapeutics.
If we moved to outcomes-based pricing then existing drugs that come to market will look for solutions to help them achieve those outcomes as part of a bundle. If a patient doesn’t take their drugs and therefore has bad outcomes, the drug companies will want to invest in tools/software/services that work in conjunction with their drugs to ensure those outcomes are met. By attaching an outcome to a bundled price, we wouldn’t have to figure out the minutiae of what counts as a digital therapeutic and instead just figure out what the package should look like that tries to target that outcomes.
I’m very curious to see how Akili chooses to price their product. How much are payers going to be willing to reimburse it? How long do patients use it before it “ends” and does Akili get paid for a fixed amount of time? Would there be discounts if patients want to continue to use the therapy? Lots of open questions here.

Pragmatic trials
One of the interesting parts of the Akili saga is that in the last few months the FDA guidance let all of these low-risk psychiatric digital therapeutics out into the real-world during COVID. After years of trying to get approval + running different clinical trials to do this Akili just…could. So they got a page up that patients could just sign up for. And very soon after they got FDA approval.
When COVID started I made some predictions about what was going to change, and one of them was the need to think about different trial designs. I hope that Akili helps usher a new era of pragmatic trials for digital therapeutics, where low-risk interventions can be released into the population, assessed in a real-world setting, and then evaluated for approval based on that data.

One of the benefits of digital therapeutics is the easy distribution, the fact that it captures data for real-world evidence naturally, and it can be modified on the fly. It would be a shame if the trial designs didn’t reflect those advantages (plus they’d be good tests for the company on the actual effectiveness and usage).
New pragmatic trials also have some other interesting byproducts.
For one, releasing a therapeutic into the wild creates consumer demand for the product. One of the main struggles digital therapeutics companies face is how to actually build up a salesforce to get doctors to prescribe them. Many have gone to traditional pharma companies to use their salesforce, but many of those deals have gone sour and honestly we haven’t seen whether or not pharma’s salesforce is actually effective at selling a digital therapeutic yet.

What if digital therapeutics have more bottoms-up adoption where this looks more like an over-the-counter nonprescription therapeutic or patients bring it up themselves to doctors? This gets into a separate conversation about the ethics of marketing therapeutics directly to patients.
Second, the line between a diagnostic and a therapeutic start blurring. One version of the game could help assess whether a child has low-grade ADHD, and transition them into the therapeutic version of the game. Plus the game is already assessing and modifying itself based on in-game performance anyway so it has to have some diagnostic properties already. If the digital therapeutics companies go up the funnel and are used for disease screening - they can own the entire loop of diagnosis-distribution-treatment-results. That also in effect helps generate demand and can also help with the sales/distribution issue.
It’s also worth noting how difficult it is to try and run a traditional clinical trial for a software-only digital therapeutic. You need to create a control arm that won’t trigger a strong placebo effect and the users think it’s the real digital therapeutic. Akili had to create a separate game which…is an increasingly more challenging version of Boggle? Honestly this could be a separate business line that I’d use…just saying.
The control was designed to match AKL-T01 on expectancy, engagement, and time on task in the form of a challenging and engaging digital word game, targeting cognitive domains not targeted by the AKL-T01 intervention and not primarily associated with ADHD. The user was instructed to find and connect letters on a grid to spell words; points are awarded on the basis of number of words formed, word length, and the use of unusual letters. There is progression in difficulty to maintain engagement and expectation of benefit from patients and their caregivers.
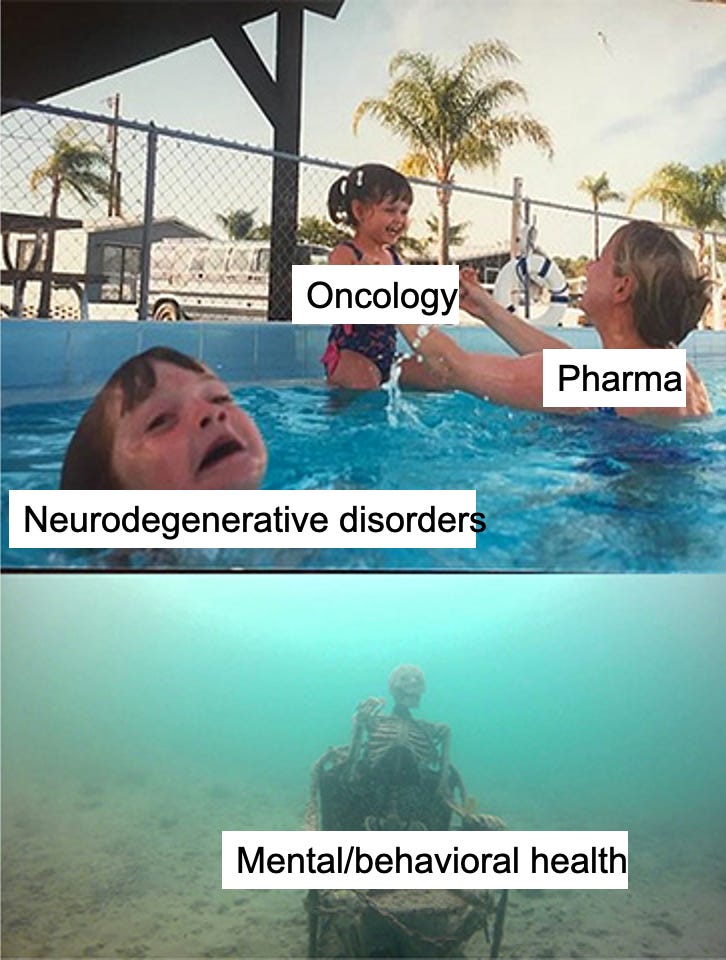
One of the reasons the pharma pipeline is so dry in areas that digital therapeutics target (low risk mental/behavioral health, neurodegenerative disorders, etc.) is because these trials are expensive to run/recruit for and it’s really hard to prove that it’s substantially better than the placebo effect when you’re targeting low-moderate severity issues. For digital therapeutics which have such a low side-effect profile, do we really need to subject them to these expensive trial designs? It would be great to incentivize more of these interventions in areas pharma has largely ignored, and pragmatic trials could be one way to do that.
And finally, how will updates work for these software-based therapeutics? One of the benefits of using software instead of a pill is that you can make modifications and updates as you learn new information. You can even test and modify “doses” per person much more easily. If Akili is being treated like a traditional therapeutic under a defined clearance for some specific endpoint, what happens if the company wants to ship updates?
Normal drugs are relatively standardized in how they’re delivered (can’t change a pill too much). Digital therapeutics have variance in how they’re delivered, either because they include services like coaching or because the algorithm tailors itself to the patient. Either the FDA has to set up rules and audits around the quality of these digital therapeutics when they’re out in the wild, or by moving to an outcomes-based pricing model the digital therapeutics companies will have to police themselves.
I’m interested to see what this relatively traditional drug clearance and trial design allows Akili to do and not to do once it hits the real world when it comes to updating and making modifications to the therapeutic.
Parting thoughts
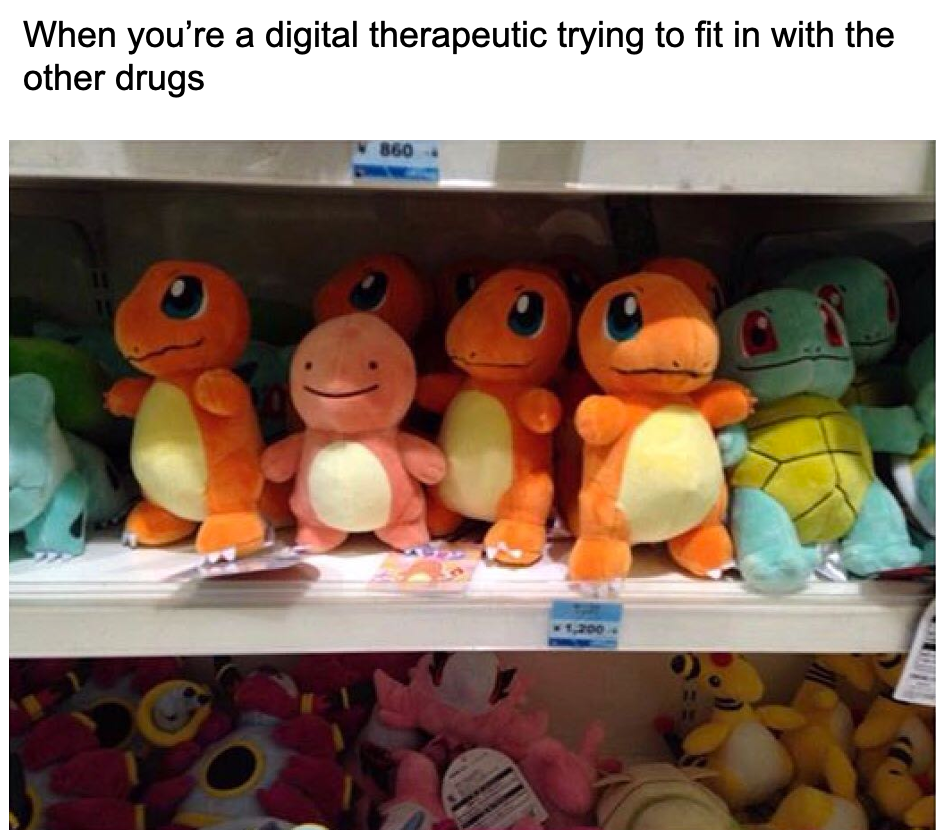
I think digital therapeutics try really hard to retrofit themselves to neatly fit into the characteristics of a traditional drug when the reality is they’re something completely. new.
If we think about this from a “jobs-to-be-done” framework, the question is how do we deliver the most cost-effective treatment to a patient based on that patient’s characteristics. That might look like coaching. That might look like a video game. That might look like a traditional drug.
The reality is right now the way reimbursement works is not amenable to that framework, which is a downside for digital therapeutics that tend to cross the lines of diagnostic, care delivery, and therapeutic. Digital therapeutics companies try to fit themselves neatly into one of these boxes for reimbursement/fundraising purposes but honestly it’s not a neat fit. The strategy and reimbursement for these companies should really be rethought from the ground up.
Some final rambling thoughts:
I think many digital therapeutics companies might not outperform a placebo, but I actually think that’s okay. The placebo effect is powerful and actually does have a strong therapeutic effect on people, but we have no ethical way of prescribing it (your doctor can’t lie and give you a sugar pill). Maybe digital therapeutics are a workaround?
How do patents work in this case? Can a digital therapeutic go “off patent”? For Akili the IP seems to be around the interface and the algorithms, but how defensible is that?
It’s cool to see gamification used in a positive way. At a time where everyone is trying to figure out how to best engage patients in their home, therapeutics that people ACTUALLY want to use seems promising. The displayed number itself then becomes an intervention - if you see your weight reduction scores + a leaderboard it might actually push you to continue treatment.
Areas where digital therapeutics seem promising: on the podcast Vijay notes that it’ll probably be in areas where the biology of the disease is not as well known (e.g. Alzheimer’s). I think it’s also interesting to think about it from where pharma isn’t focusing and where the current treatment is either non-existent or is expensive (either from a $ perspective or has a strong side effect). This is why areas like mental health and diabetes do well too.
Either way, I’m trying to see if my newsletter can be considered a digital therapeutic so if you have any ideas on what endpoint this can target let me know. Is laughter an endpoint?
Thinkboi out,
Nikhil aka. “see mom, video games were actually good”
Twitter: @nikillinit

If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.




One aspect of the open/OTC model is the potential for abuse. The regulation of the traditional therapeutic pipeline keeps quack medicine at a minimum. In a world of real world trials for digital therapeutics, what prevents game makers from taking advantage of consumers? "Farmville, now effective against diabetes."
The part of digital therapeutics I'm most interested in is the formulary and prescription aspect. Who will emerge as the FDB for digital therapeutics? Express Scripts just announced theirs in Decemver, but to be first is not necessarily a guarantee of market adoption. Who will be the Surescripts, sending prescribed digital therapeutics to app makers/consumers and enabling feedback loops (maybe Xealth)?
Has Akili published any research on long-term change in AHDH symptoms for its patients? So far I've only seen short-term results.