
Hello - lots of new faces here thanks to a throwaway joke I made after hearing the 10,000th pitch to “make a personal health record”.
The fact that this spread has confirmed two things for me:
Whoever told me to do cold emails to get sign ups does not understand the power of a dank meme game. It’s a new era baby.
I have no idea what the internet will find funny. I truly thought this was going to be too niche for anyone to like.

But I also got a lot of questions like “well why doesn’t paying for healthy behaviors work?”. So I thought I’d talk through this graphic across a couple of newsletters.
“We Should Pay People”
I don’t think anyone disagrees that many of the health issues that plague our country are generally an amalgamation of unhealthy behaviors. Poor eating habits, sleep deprivation, stress, etc. Wouldn’t it make sense to pay people small amounts today to make healthier choices so we spend less as a system in the long-term?

There are two parts of this to address.
First part, who would pay for something like this? The reflexive answer would be something like an insurance company or other payer. Like I discussed before, payers do not actually care about long-term health outcomes because you are going to switch plans before they’ll see the benefit of those healthy behaviors.
The reality is that unless you can lower the cost on some very specific health issue AND you can attribute your specific solution to improving the bottom line by $X, paying for healthy behaviors isn’t a very attractive proposition. It can work if you’re directly preventing an expensive hospital admission or convincing a patient to get a test, procedure, etc. done in a cheaper setting.
Attribution is actually one of the most difficult parts of this. You need a very tight feedback loop and an understood relationship between a behavior and an outcome. That’s why some areas where there is a willingness to pay include:
Anything diabetes management - The biomarker (blood sugar) is easy to measure, reacts very quickly to lifestyle changes, and is attributable to several diabetes-related complications if it doesn’t work.
Medication adherence for readmission prone disease areas - Congestive heart failure, COPD/Asthma, etc. require you to pick up your meds and actually take them. Many patients don’t do this because they “feel fine” and forget or they can’t pay, which leads to more acute issues down the line.
Screening for at-risk patients - For people that are at-risk of developing a disease that would be much more expensive if caught later, payers will give incentives for regular screening. Gift cards for mammographies to screen for breast cancer is one example.

Post-surgery - Hospitals get penalized if patients get re-admitted for certain diseases. Making sure patients do what they’re supposed to if they have one of these diseases is financially important for the hospital. Unsurprisingly targeting this readmission program is a common case study for adherence companies.
Getting care in a cheaper setting - Companies like SmartShopper will directly pay patients if they choose to get things like MRIs or infusions done in cheaper freestanding clinics, which can be considerably cheaper than hospitals.
Many “pay to do healthy things” initiatives target people in Medicare Advantage plans, not only because they tend to have a lot of the issues I stated above, but because Medicare Advantage is one of the few places where consumers actually shop themselves since it’s independent of their employers. If your plan doesn’t have attractive benefits, people will actually switch off (like paying you to do stuff).
In 2018, UnitedHealth decided to stop covering SilverSneakers, a fitness program for seniors. This is not a group you want to get pissed off.
Graves, who works out four to five days a week and has a UnitedHealthcare Medigap policy, decided to seek coverage elsewhere after the company raised his policy’s rates and eliminated SilverSneakers in California. He has signed up for a new policy with Blue Shield of California…
Ray Liss, who retired seven years ago, just changed over from UnitedHealthcare to a Humana Medicare supplemental policy with his wife. The loss of SilverSneakers precipitated the switch…

Even when you figure out who would actually pay, the second question is whether paying people for healthy behaviors works? Even in the article about SilverSneakers, UnitedHealthcare said <10% of people even used the service.
The evidence is mixed on whether these incentive programs work. So far data suggests that incentives to do one-time actions like get screened or sign up for a prevention program are pretty effective. But practically, catching the patient when they’re actually making that decision is very difficult. Longer term behaviors like medication adherence or keeping up with a chronic disease management program don’t show much consistency.
It’s also hard to figure out if these programs actually reduce cost to the system because it can take decades to study. There’s a lot of other variables that will impact these patients in that period and it’s difficult to tell if those same patients would have done those behaviors anyway without incentives.
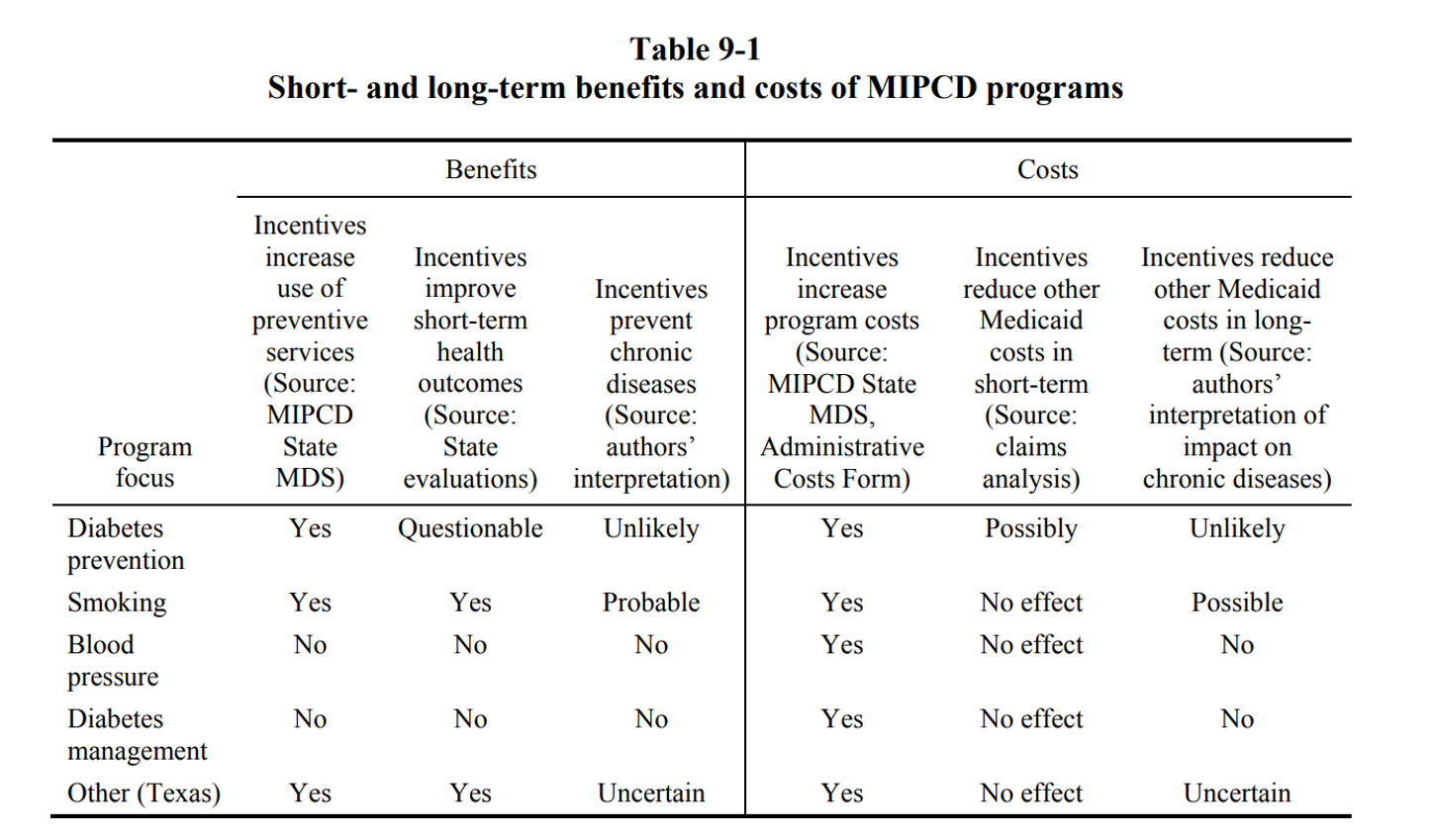
Medicaid actually has a program called Medicaid Incentives For Prevention Of Chronic Disease (or the unpronounceable MIPCD) where 10 states actually set up incentive programs for Medicaid recipients to join these healthy behavior programs like smoking cessation, diabetes prevention, diabetes management, blood pressure management, etc. The report on its cost-effectiveness is an interesting read, but generally findings suggest some short-term benefits in getting Medicaid beneficiaries to enroll in services or programs, and unclear cost savings.
But maybe these programs fail because of the incentive design itself. Giving cash to patients if they do something is a pretty blunt tool, and more likely than not each disease or behavior you want to induce will require a unique incentive scheme. This paper goes through some interesting examples from behavioral economics, e.g. for substance abused disorder, they increased medication compliance by having the reward steadily increase over time and reset to 0 if they failed.
To summarize, paying patients to do healthy things might work in some specific areas where you can prove that paying incentivized a behavior with a short-term ROI. I don’t think the idea of giving patients cash to do healthy behaviors is a bad idea - but I think it has to be extremely targeted to a specific behavior and most people who start at this proposition don’t do that. I also don’t think this is a standalone business, and is likely a feature in a larger risk-bearing entity like an insurer.
Also, honestly, this is probably a better pitch to life insurance than healthcare.
“We Need To Build A New EMR”
Inevitably when someone starts building a healthcare company, they eventually hit the same problem. All the valuable data is locked in a disparate network of Electronic Medical Records (EMR) and it’s hard to get that data out. What we need is a NEW, and better EMR.

This is a pain point in the industry, for sure. I usually see one of the following approaches.
We are going to make a personal health record directly in the hands of patients.
People in this camp usually discover that most patients actually don’t want or need their own health records because they don’t use the health system that much. Plus they don’t want to take the time to input and structure the data.
This is actually doable for motivated patients with complex care in multiple settings and have interest from life sciences, both from a clinical trial recruiting standpoint + seeing how a disease naturally progresses over time. Examples would be Ciitizen (cancer) and RDMD (rare disease), and would imagine there’s interest in the neurodegenerative and autoimmune side of things.
But for the most part, getting patients to download an app, get their existing records from multiple places, update their records, etc. is a tough sell if you’re not a regular user of the healthcare system. I basically only download new apps now because of peer pressure from my other tech friends.
We are going to make a new health record for doctors that they actually enjoy using.
People in this camp end up discovering how risk-averse hospitals/physicians are as purchasers. No one wants to learn a new EMR after learning their own. The downside risk of switching to a no-name EMR is very high. The process of switching over to a new EMR is very intensive and takes years.
Plus, it’s important to recognize the main use of an EMR is NOT being a good medical record - it’s being a good at billing for services. Good UX is not the reason people buy the tool. The purchasers (hospital administrators) and the users (physicians) are different people.
We will buy an existing EMR and re-develop/repurpose it.
This became a popular pitch after Flatiron Health bought Altos Solutions for $100M and combined it with their analytics + data structuring process to eventually sell to Roche for ~$2B. While not impossible, this is really expensive and IMO somewhat unique to the oncology space due to the prevalence of independent cancer centers, high pharma interest in oncology, and a reasonably priced option to buy with decent market share. Modernizing Medicine is another company that went down this strategy, acquiring gMed to move more into the gastroenterology field.
But honestly, if you can find someone to write you a check big enough to try this strategy, go for it. And also give me a cut or something.
We will connect data from all the existing EMRs into a single structured place

More seriously, this is doable but it’s a slog. You have to go to each provider one-by one, get an agreement, integrate with them, and then standardize/structure data. Then one of three things happens:
You can use and give de-identified patient data to third-parties, which isn’t useful if you actually want to do something that requires contacting patients directly or getting them involved in their health record.
You can use identifiable data for a specific use case that you outline with a hospital in a Business Associate Agreement (BAA). But you can’t really let other third-parties access the data that you’ve received. This is good if you want to build something specifically that benefits your company and the hospital, but doesn’t let you build a platform for third-parties to use the data or combine datasets (usually).
You get patients to give you consent to use their identifiable data for third-parties, but this requires them to actually go through the process of giving you consent. Usually this requires them logging into each EMR where they received care, but how many of you even set up an account with your EMR (let alone remember the username and password)?
This strategy sounds good in theory but is extremely slow and takes a looooong time. Apple is integrated with 474 healthcare institutions after 2-3 years, not even including the product development time leading up to the announcement. And they’re Apple, not your shitty startup with no vowels. People actually take them seriously and they have built-in distribution with the app already in millions of phones.
The other part of this that’s worth saying: despite what hospitals may say about interoperability and data sharing, they do not want patients to be easily able to take their records to a new hospital aka. have “patient leakage”. It is not their incentive to let this data out of the hospital.

Record Breaking
This makes me sound like a hater, but I actually am optimistic for a new EMR to emerge and am hopeful that it’ll happen in the next decade. Some thoughts:
ONC/HHS have established the final rules and timelines for health data to be available via API in a standardized format (only took like 12 years, smh healthcare). Though the timelines are probably messed up due to COVID, this data should actually become much more readily accessible by 2023. Even when this happens, I think we’ll discover a lot of the data in these EMRs is MEANT for billing and not a TRUE patient record. But it’ll be a good starting point, and we’ll likely see layers built on top of this.

I think a lot of the new care models focusing on customer experience may build new EMRs that do actually act as platforms. For example, One Medical built their own EMR since it was critical to the care experience. I think the wave of specialty-specific or demographic-specific care models will build versions of their own for third-parties to build on top of.
EMRs are built for a fee-for-service environment. I’m bullish on the entire payment landscape changing, either to one that places a heavier emphasis on patients paying/choosing options, and/or one with some government run payers or providers. I think a change in healthcare payment will radically change what’s needed in a medical record.
The amount of data that patients are generating outside of the hospitals via wearables, at-home diagnostics, etc. is likely to grow exponentially post-COVID as care is forcibly being pushed to home settings. This is going to increase the demand to have a patient-hub where they can view that data regularly and have it incorporated in their records. Current EMRs definitely can’t do that well, which is an open opportunity for the middle layers between the hospital EMR and wearables, like an Apple Health.
I’m still interested in middle-ware systems documentation system like voice-to-text as a tool to potentially build their own patient record. I wrote more about that here.
All-in-all, I don’t think what we currently call “Electronic Medical Records” are records at all - they are systems of billing and there’s room to actually build a new TRUE record. But don’t just “build an app a patient can input their health data into”, there needs to be some actual thought in the type of patient being targeted, the person paying for the record, and the distribution strategy.
Conclusion
To tie “paying people to do things” and “building a new EMR” into a bow - it’s worth noting that the only real reason EMRs were adopted in the first place was…because we paid hospitals to adopt them! $36B+ in total.
Here’s my pitch: What if we took another $36B (aka. ~$109 per person in America) and told everyone they’d get another $109 per person in their stimulus checks if they downloaded all of their health records into one place. What would happen???

That concludes the first two steps of the six stages of grief. Next time I’ll continue on with the rest of them.
Thinkboi out,
Nikhil aka. “Mom I’m Famous For A Meme About Healthtech Entrepreneurs!”
Twitter: @nikillinit

If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.




You had me at the Gartner hype cycle...so spot on. A lot has changed (not inside healthcare of course but outside). It would be great to debate
NIkhil, you've taken me on a real life journey back to my digital health biodesign fellowship all the way to where I am today at a large EMR company. Excellent read. I wish I had your article 3 years ago so I could have pieced together the problems I was looking into in healthcare. And yes, we pitched a life insurance company. Looking forward to reading the other posts! - Daniel